

 |  |
PREVENTING AND TREATING DEEP VEIN THROMBOSIS: Directing New Initiatives, Using New Ideas
Deep vein thrombosis (DVT) is a common and serious medical condition that affects about two million people in the United States. It occurs when a blood clot partially or completely blocks blood flow in a vein, usually in the lower legs. Risk factors include trauma, cancer, advanced age, hospitalization, surgery, and any event that keeps people off their feet for long periods.
Symptoms of DVT include pain, swelling, tenderness, or redness of the leg. However, as many as half of all episodes produce minimal symptoms, or are completely "silent." Dangers include clots breaking off and migrating to the lungs, leading to life-threatening pulmonary embolism (PE).
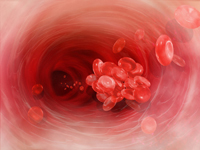
![]() The mainstay therapy for DVT has been anticoagulation for many years. Anticoagulation helps prevent propagation of thrombus (blood clots) and decrease the risk of pulmonary embolus, but has little effect on the long-term complications.
The mainstay therapy for DVT has been anticoagulation for many years. Anticoagulation helps prevent propagation of thrombus (blood clots) and decrease the risk of pulmonary embolus, but has little effect on the long-term complications.
Long-term complications of DVT include chronic leg pain, swelling, and skin changes. The signs and symptoms are described as post-thrombotic syndrome. In its advanced stage, patients may develop venous leg ulcers (open sores). These complications cause significant physical and emotional distress, as well as a financial burden on our society.
In July 2008, the American College of Chest Physicians released new evidence-based clinical guidelines for the prevention and treatment of DVT and PE. These guidelines recommend that early thrombus removal be offered to patients with extensive proximal acute DVT who are good candidates.
In September, the U.S. Surgeon General, Rear Admiral Steven K. Galson, MD, MPH, issued an official "Call to Action" — only the seventh issued in the past 11 years from the Office of the Surgeon General — to reduce the number of cases of DVT and PE in the United States.
This "Call to Action" includes the need to create evidence-based practices for DVT/PE prevention, diagnosis, and treatment. Hospitals and physicians are required to develop DVT protocols to prevent and treat DVT/PE.
LEADING THE WAY TO BETTER CARE
Our Division of Vascular Surgery has been leading the efforts at Stony Brook University Medical Center to prevent and treat DVT/PE. A multi-specialty DVT team has been formed to create a hospital-wide program for patient assessment and DVT prophylaxis.
The goal of this team is to dramatically reduce the incidence of hospital-acquired DVT, and to provide the most advanced treatment options to patients with DVT.
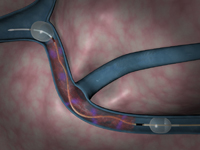
![]() At Stony Brook, patients with DVT are treated by our vascular team, and offered a minimally invasive procedure. Use of thrombolytics (clot-disrupting drugs) with the combination of mechanical thrombolytic devices, such as the Trellis-8 or Angiojet device, allows us to mechanically disrupt and remove the clot.
At Stony Brook, patients with DVT are treated by our vascular team, and offered a minimally invasive procedure. Use of thrombolytics (clot-disrupting drugs) with the combination of mechanical thrombolytic devices, such as the Trellis-8 or Angiojet device, allows us to mechanically disrupt and remove the clot.
These medical devices decrease the treatment time and the amount of thrombolytics used, thus decreasing the bleeding risk and hospital stay. In about two-thirds of patients, the procedure can be performed in a single setting with the patient going home the next day.
Early treatment with removal of clot helps reduce the risk of recurrent thrombosis, and reduces the risk of vein valve damage. This results in prevention of the long-term complications of post-thrombotic syndrome.
Our vascular team has been following patients treated with thrombolysis over the last five years to evaluate the mid-term results.
Antonios P. Gasparis, MD, assistant professor of surgery and director of the Stony Brook Vein Center, presented our findings at the 2007 annual meeting of the American Venous Forum, and the paper reporting them has been accepted for publication in the Journal of Vascular Surgery.
Our data demonstrate that good early clinical results after pharmaco-mechanical thrombolysis can be sustained on longer follow-up, and may prevent the development of advanced post-thrombotic syndrome.
 For consultations/appointments with our vein specialists, please call 631-444-VEIN (8346).
For consultations/appointments with our vein specialists, please call 631-444-VEIN (8346).

| Back to Departmental News | Return to Home Page |