

 |
 |
DEPARTMENT OF SURGERY [See "History of Department"]
The Department of Surgery is made up of eight clinical divisions and one clinical group that represent diverse areas of surgical specialization, plus an education division, all of which are described below. The Department's full-time clinical faculty are responsible for the care of patients and the instruction of residents both at Stony Brook University Medical Center and the Northport Veterans Affairs Medical Center. The Department, under the direction of Dr. Todd K. Rosengart who is chairman, provides an academic and administrative umbrella over all the activities of the residency program.
Breast Surgery Division
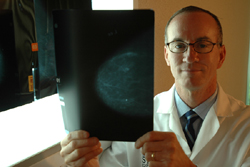
![]() The Breast Surgery Division is responsible for the care of patients with breast cancer. It runs the multidisciplinary breast service at our state-of-the-art Carol M. Baldwin Breast Care Center, which in 2009 was granted a full three-year accreditation by the National Accreditation Program for Breast Centers (NAPBC). The NAPBC is a new program administered by the American College of Surgeons, and our breast center is the first in New York State to gain this elite designation.
The Breast Surgery Division is responsible for the care of patients with breast cancer. It runs the multidisciplinary breast service at our state-of-the-art Carol M. Baldwin Breast Care Center, which in 2009 was granted a full three-year accreditation by the National Accreditation Program for Breast Centers (NAPBC). The NAPBC is a new program administered by the American College of Surgeons, and our breast center is the first in New York State to gain this elite designation.
The breast surgery service is covered by a PGY-2 surgical resident. This resident is responsible for all service-related issues. The educational focus is on the initial work-up, diagnosis, and management of breast abnormalities. There is extensive operating room experience, as well. There is major emphasis on the multidisciplinary approach to breast cancer treatment. Participation in lectures and the weekly multidisciplinary breast conference is required.
Our weekly treatment planning conference is a multidisciplinary forum where we review potential treatment options for patients with newly diagnosed cancer or patients with recurrent disease. At this conference, their individual cases are presented to a team of highly trained cancer specialists, including radiologists, breast surgeons, pathologists, reconstructive surgeons, radiation oncologists, and medical oncologists. Indeed, our multidisciplinary team approach to breast cancer treatment distinguishes the quality of care we provide for our patients.
Click here to see selected publications by faculty in this division.
Cardiothoracic Surgery Division
![]() The Cardiothoracic Surgery Division manages the most active clinical service in the Department. Currently, this service performs annually 500 adult open-heart procedures and 150 adult thoracic procedures. This is not simply a coronary service: the resident is introduced to the whole spectrum of cardiopulmonary surgery, including neonatal, valve reconstructive, electrophysiological, videothoracoscopic, and thoracic aortic surgery. Third- and fourth-year residents participate in these operations, and with a second-year resident, run University Medical Center's 10-bed cardiovascular intensive care unit, which is capable of providing postoperative care for the highest-risk heart patients.
The Cardiothoracic Surgery Division manages the most active clinical service in the Department. Currently, this service performs annually 500 adult open-heart procedures and 150 adult thoracic procedures. This is not simply a coronary service: the resident is introduced to the whole spectrum of cardiopulmonary surgery, including neonatal, valve reconstructive, electrophysiological, videothoracoscopic, and thoracic aortic surgery. Third- and fourth-year residents participate in these operations, and with a second-year resident, run University Medical Center's 10-bed cardiovascular intensive care unit, which is capable of providing postoperative care for the highest-risk heart patients.
The aim of the general surgery resident rotations on the cardiothoracic service is to formulate a solid foundation in cardiopulmonary physiology and medicine, to learn and perform thoracic surgical incisions, to develop a practiced understanding of vascular surgical principles, and to gain confidence when working around the heart and great vessels, particularly in trauma situations. Ample opportunity is afforded to gain experience and understanding in bronchoscopy, cardiac catheterization and angiography, the heart-lung machine, and the intra-aortic balloon pump.
One of four graduating residents in the general surgery program, during the last six years, has chosen to pursue fellowship training in cardiothoracic surgery, and they have matriculated at programs at top institutions that include New York University, University of Alabama-Birmingham, Texas Heart Institute, Case Western Reserve University, University of Rochester, and Tufts University.
Cardiac surgical conferences are held each week, in addition to a biweekly cardiac surgery seminar. The division has three ongoing databases to facilitate clinical research, and ongoing projects in homograft vein bypass's, cardiovascular accident prediction and prevention, and papillary muscle resuspension. Among current research projects are: angioscopic adjuncts to coronary artery surgery; myocardial mechanics and energetics; myocardial protection by cardioplegia; new endogenous myoprotective strategies utilizing preconditioning, and immunomodulation during cardiopulmonary bypass. Resident participation in the division's research activities on a formal or informal basis is encouraged, and several residents have presented their findings at national meetings.
Click here to see selected publications by faculty in this division.
Colon and Rectal Surgery Division
Chief, Roberto Bergamaschi, MD, PhD

![]() The Colon and Rectal Surgery Division is responsible for the care for patients with a wide range of diseases and disorders of the small bowel, colon, rectum, and anus. These include colon, rectal, and anal cancer, diverticulitis, familial polyposis, ulcerative colitis, Crohn's disease, ileoanal reservoir (J-pouch), colon polyps, incontinence, prolapse, anorectal abscess, fistula, fissure, and hemorrhoids.
Our colorectal faculty has broad expertise in the entire spectrum of colon and rectal surgical procedures, including minimally invasive surgery (laparoscopy) and other minimally invasive procedures for the treatment of colorectal diseases. They are skilled at performing sphincter-sparing surgery in the treatment of rectal cancer, which spares patients the inconvenience and emotional burden of a colostomy bag. They are also committed to performing colon cancer screening, and perform colonoscopy, among other diagnostic tests. For the management of fecal incontinence, treatment options include the new Secca procedure, artificial anal sphincter, and muscle transplant.
The Colon and Rectal Surgery Division is responsible for the care for patients with a wide range of diseases and disorders of the small bowel, colon, rectum, and anus. These include colon, rectal, and anal cancer, diverticulitis, familial polyposis, ulcerative colitis, Crohn's disease, ileoanal reservoir (J-pouch), colon polyps, incontinence, prolapse, anorectal abscess, fistula, fissure, and hemorrhoids.
Our colorectal faculty has broad expertise in the entire spectrum of colon and rectal surgical procedures, including minimally invasive surgery (laparoscopy) and other minimally invasive procedures for the treatment of colorectal diseases. They are skilled at performing sphincter-sparing surgery in the treatment of rectal cancer, which spares patients the inconvenience and emotional burden of a colostomy bag. They are also committed to performing colon cancer screening, and perform colonoscopy, among other diagnostic tests. For the management of fecal incontinence, treatment options include the new Secca procedure, artificial anal sphincter, and muscle transplant.
Our state-of-the-art Anorectal Physiology Laboratory provides advanced diagnostic capabilities, and serves as a strong educational resource for residents. Our new Clinical Skills Center offers residents essential training experience by means of surgical simulation of laparoscopic colorectal surgery. (See Stony Brook study abstract to be presented at 2009 Annual Meeting of the American Society of Colon and Rectal Surgeons: "Simulated Laparoscopic Sigmoidectomy Training: Responsiveness of Surgery Residents.")
The Colon and Rectal Surgery Division offers an independent, accredited one-year colon and rectal surgery residency. This clinical residency is designed to prepare the surgeon for the pursuit of an academic career in colon and rectal surgery equally as well as for private practice as a colon and rectal surgeon. The content of the educational experience is directed toward fulfilling the requirements of the American Board of Colon and Rectal Surgery. Residents gain operative experience through a large volume of diverse surgical procedures, including reconstructive anorectal surgery, surgery for inflammatory bowel disease, emergency colon resections, ambulatory anorectal surgery, and all aspects of office and endoscopic procedures.
Click here to see selected publications by faculty in this division.
Education Division
Director, Joseph J. Sorrento, Jr., MD

![]() The Education Division was established to reaffirm the Department’s dedication to the ideal that the primary goals of a university-based teaching hospital must include an unwavering commitment to the education of both medical students and residents. We further recognize that the challenge of the new century is to teach a greatly expanded knowledge base with less time to teach it. The methodology of the past — in which the emphasis has been on what is taught rather than what is learned; the teacher has been the active dispenser of knowledge and the learner the passive recipient; and the teacher, rather than the learner, has set the learning agenda — makes less and less sense today.
The Education Division was established to reaffirm the Department’s dedication to the ideal that the primary goals of a university-based teaching hospital must include an unwavering commitment to the education of both medical students and residents. We further recognize that the challenge of the new century is to teach a greatly expanded knowledge base with less time to teach it. The methodology of the past — in which the emphasis has been on what is taught rather than what is learned; the teacher has been the active dispenser of knowledge and the learner the passive recipient; and the teacher, rather than the learner, has set the learning agenda — makes less and less sense today.
To maintain the educational excellence that has been a tradition of the Department since its founding in 1974, the Education Division is committed to providing learner-centered education in which the resident helps to establish how he or she can best learn, with the faculty increasingly serving as facilitators of self-education.
Our educational programs emphasize interactive teaching in a case-based format. We provide web-based interactive learning programs that supplement the classroom lectures. With the realization that effective teachers are made and not born, we have endeavored to improve our teaching by enhancing faculty development efforts; to increase faculty insight into their own teaching attributes, we have improved and expanded our feedback tools. To facilitate communication, we have greatly expanded our mentoring program. To help prepare physicians for the medical challenges of the future, we have redoubled our efforts to train our residents as future clinical investigators by increasing opportunities for them to gain research experience.
General Surgery, Trauma, Surgical Critical Care, and Burns Division
Interim Chief, Marc J. Shapiro, MD
The General Surgery, Trauma, Surgical Critical Care, and Burns Division comprises four clinical sections, each of which offers residents a broad range of clinical experience as well as academic programs and research opportunities:
General Surgery Section

![]() An extremely active general surgery exposure is assured from the simple to the most complex of disease states, with a majority of them requiring one and, on occasion, multiple surgical interventions. Providing state-of-the-art surgery, this section gives residents unique opportunities for exposure ranging from advanced laparoscopic procedures (see Center for Minimally Invasive Surgery) to major abdominal wall reconstruction and major hepatobiliary procedures. Complex conditions and patients with complications are referred to the General Surgery Section from a wide geographic region for specialization in all aspects of general surgery provided at Stony Brook University Medical Center. The resident participates in the office setting for patient interaction including preoperative and postoperative care and evaluation, in addition to the perioperative care delivered in the hospital and in the operating room.
An extremely active general surgery exposure is assured from the simple to the most complex of disease states, with a majority of them requiring one and, on occasion, multiple surgical interventions. Providing state-of-the-art surgery, this section gives residents unique opportunities for exposure ranging from advanced laparoscopic procedures (see Center for Minimally Invasive Surgery) to major abdominal wall reconstruction and major hepatobiliary procedures. Complex conditions and patients with complications are referred to the General Surgery Section from a wide geographic region for specialization in all aspects of general surgery provided at Stony Brook University Medical Center. The resident participates in the office setting for patient interaction including preoperative and postoperative care and evaluation, in addition to the perioperative care delivered in the hospital and in the operating room.
As a tertiary referral center, hepatobiliary disease, pancreatic disease, inflammatory bowel disease, gastrointestinal bleeding, and upper/lower endoscopic interventions are referred with regularity. State-of-the-art videoscopic equipment as well as wet labs provide excellent clinical experience. The development of a gastrointestinal center of excellence and expertise in foregut surgery offers residents opportunities to participate and experience the most current surgical techniques available. Clinical research is ongoing and basic science research is available. There is a large degree of attending surgeon interaction in addition to a number of conferences focused on issues related to general surgery, such as morbidity and mortality, resident clinical education conference, tumor board, GI conference, and others. There is an advanced laparoscopic fellowship offered for postgraduate surgical trainees as well.
Trauma Section

![]() As the only Level I Trauma Center designated by the State of New York for Suffolk County, University Medical Center provides all aspects of trauma care. It is the only facility serviced by air ambulances in the county. With over 1,600 trauma admissions and twice as many seen and discharged from an emergency room with over 75,000 annual visits, the trauma team is one of the most visible groups within the medical center. Stony Brook University Medical Center serves as EMS medical control for the entire county for ground and air ambulances, and has a mobile ICU on site.
As the only Level I Trauma Center designated by the State of New York for Suffolk County, University Medical Center provides all aspects of trauma care. It is the only facility serviced by air ambulances in the county. With over 1,600 trauma admissions and twice as many seen and discharged from an emergency room with over 75,000 annual visits, the trauma team is one of the most visible groups within the medical center. Stony Brook University Medical Center serves as EMS medical control for the entire county for ground and air ambulances, and has a mobile ICU on site.
Resident education begins with advanced cardiac life support (ACLS) and advanced trauma life support (ATLS) courses during orientation. Based on resident input and attending involvement, the night float service serves as the core trauma service with a senior or chief resident, assistant residents, interns, and medical students rounding out the team. The trauma team is responsible for patient care in the emergency room, and is notified on the basis of a three-tiered response system, depending upon the severity of patient injury. An up-to-date trauma manual for the Stony Brook Trauma Center is provided for each participant of the trauma team. Aggressive resuscitation, procedures, both major and minor-including resuscitative thoracotomy and patient care plans are carried out in the emergency room and usually in the shock-trauma bay which consists of eight resuscitative beds.
Radiographic machines, including a computed tomography scanner, are available in the emergency department, which is undergoing major reconstruction for a continued state-of-the-art center. The operating rooms are adjacent to the emergency deartment, providing easy access for facile care. The attending traumatologists are dedicated and trained to provide all aspects of care, from the surgical to the critical care components. Attending rounds including teaching rounds are carried out daily to provide optimal education and patient care. The trauma clinic is attended to by all day members of the team which includes the attending, assistant residents, interns, medical students, and physician assistants. The trauma team manages all surgical related issues for their ICU patients.
The trauma research laboratory is actively involved in shock and hypoxia research, presenting at national meetings regularly and publishing in peer review journals Ongoing clinical research in all aspects of care is ongoing and focuses on shock, hypoxia, anemia, blood substitutes, antibiotic therapy for sepsis and soft tissue infections, laparoscopy and the use of various hemostatic agents. There is a weekly trauma conference that includes morbidity and mortality, didactic and research presentations and discussion of system issues. The regional trauma committee is also coordinated through Stony Brook as well.
The Trauma Section presents to a senior (fourth-year) surgical resident the annual David J. Kreis Jr. Award for Excellence in Trauma Surgery.
Surgical Critical Care Section

![]() A 20-bed state-of-the-art surgical intensive care unit provides the highest level of care possible. Directed by a surgical intensivist, this multidisciplinary critical team is primarily responsible for all patients in the SICU, co-managing the patients with the primary service. The SICU team consists of an intensivist in the Department of Surgery or Anesthesiology, a nurse practitioner and assistant residents from surgery, anesthesia, emergency medicine and obstetric-gynecology, providing around-the-clock care. All aspects of monitoring and procedures are performed in the SICU, such as percutaneous tracheostomies, esophago-gastro-duodenoscopy (EGD) with percutaneous endoscopic gastrostomy (PEG) tube placement, pulmonary artery placement, transesophogeal doppler monitoring, and bispectral index (BIS) monitoring, as well as aggressive resuscitation and utilization of a wide range of inotropic and chronotropic support. A handbook is distributed to all members of the team in addition to orientation when the team rotates into the SICU.
A 20-bed state-of-the-art surgical intensive care unit provides the highest level of care possible. Directed by a surgical intensivist, this multidisciplinary critical team is primarily responsible for all patients in the SICU, co-managing the patients with the primary service. The SICU team consists of an intensivist in the Department of Surgery or Anesthesiology, a nurse practitioner and assistant residents from surgery, anesthesia, emergency medicine and obstetric-gynecology, providing around-the-clock care. All aspects of monitoring and procedures are performed in the SICU, such as percutaneous tracheostomies, esophago-gastro-duodenoscopy (EGD) with percutaneous endoscopic gastrostomy (PEG) tube placement, pulmonary artery placement, transesophogeal doppler monitoring, and bispectral index (BIS) monitoring, as well as aggressive resuscitation and utilization of a wide range of inotropic and chronotropic support. A handbook is distributed to all members of the team in addition to orientation when the team rotates into the SICU.
Stony Brook's ACGME-accredited surgical critical care residency (fellowship) program is one of the few in the United States, and fills its two allotted spots without difficulty. There are detailed daily attending bedside rounds and also a procedure team to aid in the care of this high acuity SICU. Procedures such as central line placement, arterial line placement, and tube thoracostomies and thoracocentesis are performed at the bedside. The ability to read online labs and radiographs facilitates patient care. There is an SICU curriculum of didactic presentations that the resident participates in, allowing the team to become comfortable to address all aspects of medical and surgical issues in this diverse population. The attendings are all experienced and trained in critical care, with a focus on the surgical patient.
Overlapping with the Trauma Section basic science and clinical research protocols, there are dedicated research clinical associates to aid with the bedside protocols. The multidisciplinary rounds include the medical team, nursing team, pharmacist, respiratory therapist, physical therapist, occupational therapist, speech pathology, psychiatric support, social service, and nutritional support. The residents participate in the weekly SICU conference as well as their specialty conferences.
Burns Section

![]() The only burn unit in Suffolk County, the Stony Brook University Burn Center is a multidisciplinary, state-of-the-art burn unit consisting of
eight beds. It admits more than 100 patients each year including inhalational injury, hyperthermia, hypothermia, and chemical and drug-induced burns. Approximately one third of the patients are in the pediatric age group. The multidisciplinary care begins in the emergency room with the physicians and nurses rapidly coordinating and providing the much-needed attention and care. Once in the Burn Center, physical therapists, occupational therapists, speech pathology, dieticians, respiratory therapists, psychiatric support, and social service assist the medical team.
The only burn unit in Suffolk County, the Stony Brook University Burn Center is a multidisciplinary, state-of-the-art burn unit consisting of
eight beds. It admits more than 100 patients each year including inhalational injury, hyperthermia, hypothermia, and chemical and drug-induced burns. Approximately one third of the patients are in the pediatric age group. The multidisciplinary care begins in the emergency room with the physicians and nurses rapidly coordinating and providing the much-needed attention and care. Once in the Burn Center, physical therapists, occupational therapists, speech pathology, dieticians, respiratory therapists, psychiatric support, and social service assist the medical team.
The ultimate goal is to assist the patient to total independence. In addition to aggressive resuscitation and airway control, all operative interventions are performed by the Burn Center team at the bedside and in the operating room. Active clinical and basic science research includes the use of culturing and growing human skin and the development of a unique living skin bank.
The resident staff actively participates in obtaining specialized training in the care of these complex patients. Initial assessment, resuscitation, administration of critical care, and surgical management are included in the educational process, as well as attending the outpatient burn clinic.
Click here to see selected publications by faculty in this division.
Otolaryngology–Head and Neck Surgery Division
The Otolaryngology–Head and Neck Surgery Division is responsible for the treatment of adult and pediatric patients with disorders of the ear, nose and throat. In addition to management of routine ENT problems, our staff has specialty interest in laryngology, including the multidisciplinary assessment and treatment of voice and swallowing disorders. Our Head and Neck Surgical team manages endocrine and oncologic disease utilizing state of the art minimally invasive techniques. Our neurotologist manages all aspects of adult and pediatric ear disease including vertigo and dizziness, hearing loss, skull base tumors and the treatment of chronic infection and cholesteatoma. Our rhinologist manages complex sinus and anterior skull base disease. Research interests in the division include the identification of molecular markers/triggers for head and neck cancer, the application of patient centered care techniques in the management of chronic otolaryngologic illness, oropharyngeal cancer screening using endoscopic confocal microscopy, and the development of novel approaches to skull base disease.
The Otolaryngology–Head and Neck Surgery Division also houses the Speech, Language and Hearing Program. This program serves as an additional point of entry to the service delivery system of University Medical Center, and its team works closely with the otolaryngological surgeons, to meet audiologic needs (hearing evaluation—including brainstem testing—and rehabilitation). In addition, speech and voice evaluation and treatment services are provided. Neurologic, physiologic and functional speech, hearing and language disabilities are also seen on referral from medical staff.
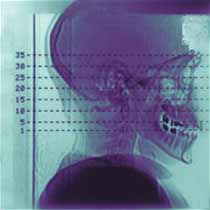
![]() The Otolaryngology–Head and Neck Surgery Division is responsible for the treatment of patients with a wide variety of head and neck disorders at both University Medical Center and the Northport VA Medical Center. A multidisciplinary approach to the treatment of head and neck tumors is followed. All patients are discussed at a biweekly teaching conference attended by interdepartmental staff with expertise in therapeutic radiology, medical oncology, oral surgery, general surgery, and otolaryngology–head and neck surgery. This teaching conference provides an excellent opportunity for the training of residents in the diagnosis and treatment of disorders of the head and neck region with special emphasis on benign and malignant tumors. An active educational program focuses on bedside rounds, operating room teaching and didactic teaching in the form of lectures and conferences.
The Otolaryngology–Head and Neck Surgery Division is responsible for the treatment of patients with a wide variety of head and neck disorders at both University Medical Center and the Northport VA Medical Center. A multidisciplinary approach to the treatment of head and neck tumors is followed. All patients are discussed at a biweekly teaching conference attended by interdepartmental staff with expertise in therapeutic radiology, medical oncology, oral surgery, general surgery, and otolaryngology–head and neck surgery. This teaching conference provides an excellent opportunity for the training of residents in the diagnosis and treatment of disorders of the head and neck region with special emphasis on benign and malignant tumors. An active educational program focuses on bedside rounds, operating room teaching and didactic teaching in the form of lectures and conferences.
In the head and neck clinic, residents are instructed in the methods used in performing a comprehensive head and neck physical examination. The differential diagnosis and therapeutic plan are discussed with the attending physician who supervises at clinic sessions. In the operating room, the residents perform and assist at a variety of head and neck surgical procedures with a special emphasis on intricate oblative and reconstructive surgery for head and neck cancer. Residents have the opportunity to utilize the latest of surgical equipment, including flexible and ridged fiberoptic instrumentation, carbon dioxide surgical laser, and the operating microscope.
The mission of the Otolaryngology–Head and Neck Surgery Division is to provide a comprehensive service for patients of University Hospital and to offer a range of clinical experience for residents and fellows at Stony Brook. Laboratory programs are currently being developed in the Health Sciences Center for a full complement of clinical and basic scientific studies including temporal bone analysis. A number of specialty clinics dealing with a wide variety of problems have been established.
Click here to see selected publications by faculty in this division.
Pediatric Surgery Division

![]() The Pediatric Surgery Division manages an active clinical service. Residents assigned to the pediatric surgery service, during their general surgery rotations, participate in the preoperative, operative, and postoperative care of general surgical, thoracic, and endoscopic problems in children ranging from premature infants through adolescents. This service also provides residents with experience in the ambulatory care unit of University Medical Center as well as the neonatal intensive care unit, pediatric intensive care unit, pediatric acute care unit, and Burn Center. Close association with the Department of Pediatrics and concurrent patient management are stressed.
The Pediatric Surgery Division manages an active clinical service. Residents assigned to the pediatric surgery service, during their general surgery rotations, participate in the preoperative, operative, and postoperative care of general surgical, thoracic, and endoscopic problems in children ranging from premature infants through adolescents. This service also provides residents with experience in the ambulatory care unit of University Medical Center as well as the neonatal intensive care unit, pediatric intensive care unit, pediatric acute care unit, and Burn Center. Close association with the Department of Pediatrics and concurrent patient management are stressed.
General surgery residents at the second- and fourth-year levels rotate through the service. A pediatric resident may also be a member of the team. Newborn congenital anomalies, pediatric tumors, and trauma constitute the most demanding areas of surgical care. Inguinoscrotal abnormalities and diseases producing intestinal obstruction, bleeding, or inflammation provide a good educational exposure for the resident. The general surgery resident is expected to learn the management of common pediatric surgical diseases and to improve his or her technical skills and surgical background by involvement with specialized index cases.
Click here to see selected publications by faculty in this division.
Plastic and Reconstructive Surgery Division
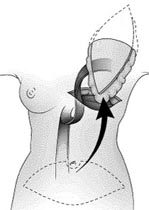
![]() The Plastic and Reconstructive Surgery Division provides reconstructive and aesthetic surgery for the care of both children and adults. Problems commonly managed are congenital anomalies of the head and neck, particularly cleft lip and palate, cancer of the head and neck requiring excision and reconstruction, injuries of the hand, deformities following burns, trunk and lower extremity deformities, and body-image problems necessitating aesthetic surgery. Conventional surgical approaches, as well as microsurgical techniques, are used.
The Plastic and Reconstructive Surgery Division provides reconstructive and aesthetic surgery for the care of both children and adults. Problems commonly managed are congenital anomalies of the head and neck, particularly cleft lip and palate, cancer of the head and neck requiring excision and reconstruction, injuries of the hand, deformities following burns, trunk and lower extremity deformities, and body-image problems necessitating aesthetic surgery. Conventional surgical approaches, as well as microsurgical techniques, are used.
Members of this division direct an active clinical program in reconstructive microsurgery at University Medical Center, and specialize in microsurgical reconstructive operations involving free-tissue transfers used for some of the most clinically vexing problems that, until recently, were virtually unsolvable. Residents have the opportunity to learn current approaches and techniques in plastic and reconstructive surgery. The Plastic Surgery Indications Conference, held once a month, further enhances our residents' educational experience in this subspecialty.
Click here to see selected publications by faculty in this division.
Upper Gastrointestinal and General Oncologic Surgery Group
![]() The Upper Gastrointestinal and General Oncologic Surgery Group is responsible for the care of patients with upper gastrointestinal malignancies, soft tissue sarcomas, and melanoma. Residents assigned to rotations on this oncology service participate in the preoperative evaluation and diagnosis of patients with various types of tumors. Residents participate in the staging, planning, and implementation of multimodality therapy, as well as the performance of definitive cancer operations including extensive exenterative resections. Postoperative management, rehabilitation, selection of patients for adjuvant therapy, and follow-up are additional important aspects of cancer management in which residents are expected to participate.
The Upper Gastrointestinal and General Oncologic Surgery Group is responsible for the care of patients with upper gastrointestinal malignancies, soft tissue sarcomas, and melanoma. Residents assigned to rotations on this oncology service participate in the preoperative evaluation and diagnosis of patients with various types of tumors. Residents participate in the staging, planning, and implementation of multimodality therapy, as well as the performance of definitive cancer operations including extensive exenterative resections. Postoperative management, rehabilitation, selection of patients for adjuvant therapy, and follow-up are additional important aspects of cancer management in which residents are expected to participate.
In the overall care of patients with cancer, our surgical oncology team works closely with the attending staff of several other departments and divisions, including medical oncology, radiation oncology, pathology, radiology, gastrointestinal medicine, and gynecologic oncology. There are numerous teaching conferences concerned with oncology, among which are the surgical oncology rounds, multimodality tumor board, and mammographic-pathologic correlation conference. As patients treated by the surgical oncology team have the opportunity to participate in national cooperative clinical trials, residents are able to gain an especially broad experience in the management of patients with cancer.
Faculty of this oncology group are national leaders in minimally invasive laparoscopic surgery for complex GI tumors (for example), including robotic surgery, and residents are able to gain knowledge and experience with these leading-edge therapeutic modalities.
Click here to see selected publications by faculty in this division.
Vascular Surgery Division
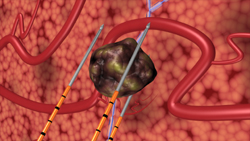
![]() The Vascular Surgery Division is responsible for the treatment of patients with a wide variety of vascular disorders, at both University Medical Center (see Vascular Center) and the Northport VA Medical Center. Between the two institutions more than 400 major reconstructive procedures are performed each year, including aortic, renal mesenteric, extracranial cerebral vascular, and peripheral arterial reconstruction. The Vascular Surgery Division is also responsible for the care of patients with portal hypertension as well as the maintenance of angio access for two large dialysis centers. Numerous other procedures such as amputation, muscle flaps, venous reconstruction, and skin grafting procedures necessary for the total care and rehabilitation of patients suffering from vascular-related diseases are also performed by the Vascular Surgery Division.
The Vascular Surgery Division is responsible for the treatment of patients with a wide variety of vascular disorders, at both University Medical Center (see Vascular Center) and the Northport VA Medical Center. Between the two institutions more than 400 major reconstructive procedures are performed each year, including aortic, renal mesenteric, extracranial cerebral vascular, and peripheral arterial reconstruction. The Vascular Surgery Division is also responsible for the care of patients with portal hypertension as well as the maintenance of angio access for two large dialysis centers. Numerous other procedures such as amputation, muscle flaps, venous reconstruction, and skin grafting procedures necessary for the total care and rehabilitation of patients suffering from vascular-related diseases are also performed by the Vascular Surgery Division.
General surgery residents rotate on the vascular services as junior residents and return again during their fourth or fifth years. In senior years, the resident is expected to obtain a good deal of operative experience. While the Vascular Surgery Division offers an ACGME-accredited residency (fellowship) in vascular surgery, the senior chief resident does not rotate on the same service with the fellow; thus, the vascular fellow in no way diminishes the surgical responsibility of the general surgery resident on the vascular services. The goals of teaching residents, at all levels, the care of patients with vascular disease are met through teaching in the form of lectures and conferences, as well as at the bedside and in the operating room.
The Non-Invasive Vascular Laboratory houses a wide variety of up-to-date equipment, including Duplex scanners and transcranial Doppler units, used not only as aids in the diagnosis of circulatory disorders, but also in the follow-up of a large number of outpatients. The Noninvasive Vascular Laboratory is complemented by an excellent special procedures division of the Department of Radiology, which likewise has the latest in angiography equipment and CT scanners, at both University Medical Center and the Northport VA Medical Center. The special procedures division provides service in all the techniques of interventional radiology, including balloon dilatation, invasive pressure monitoring and therapeutic embolization.
General surgery residents also gain experience in vascular surgery during their rotation on the vascular surgery service at Winthrop-University Hospital. This service, under the direction of Dr. George L. Hines, does a high volume (about 500 cases per year) of vascular surgery, including both categories I and II cases.
The Vascular Surgery Division will continue to grow and expand its scope of diagnosis and treatment of circulatory disorders. The general surgery resident is expected to obtain a good understanding of the physiology and pathophysiology of the vascular system and to become familiar with the techniques of vascular reconstructive surgery.
Click here to see selected publications by faculty in this division.

| Return to Department of Surgery | Return to Residency Program |